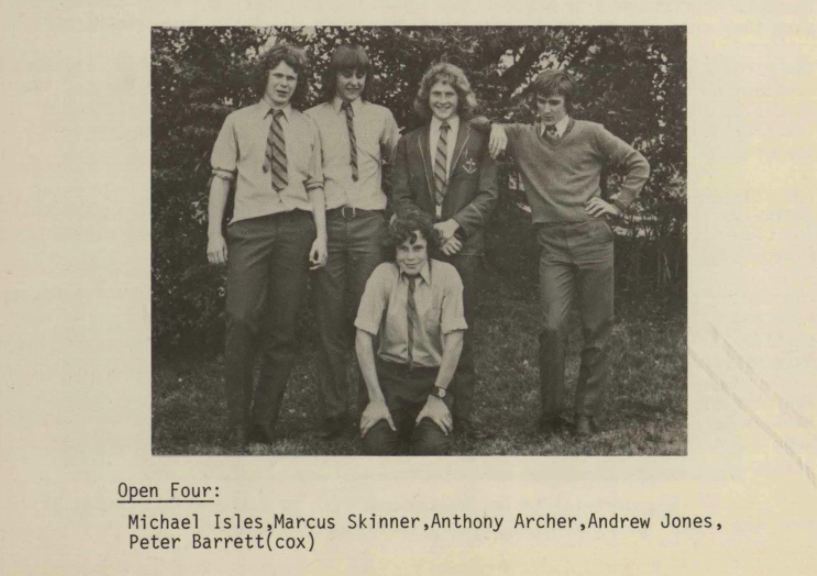
Clinical Associate Professor Marcus Skinner AM | Class of 1974
Posted on July 24, 2020
Tell us about your time at Friends’?
My family returned to Tasmania in 1971 and I commenced school life at Friends’ as a boarder in Year 9. My mother died when I was 10 and my father and step-mother wanted a stable and sound education for me. In that era the boarding house was in Carr Street with the dining room being Hodgkin Hall. Bill Oats was the headmaster at first, followed by Rod Grosvenor in 1973. At school we were required to participate in a range of activities and I remember getting up super early for rowing training and our cooked breakfast on return. As boarders we were a rowdy bunch but there were set routines and expectations of us. After dinner in the evenings we had a dedicated study time which helped establish great routines for the future. I remember well that on Sundays we would visit various religious centres in Hobart such as the Catholic and Anglican Cathedrals, Jewish Synagogue etc, but I always returned to the feeling that the Quaker values truly represented my beliefs. Looking back, Friends’ was a great environment for a young man to grow and strengthen core values. Instilled by my family, these values were cemented by the Friends’ community. My best mates were all Boarders. We had a shared camaraderie and looked out for one another because we were Boarders. Andrew Jones (Cook), Kim Frankcombe (Luigi) and Jim Roberts-Thomson (Moon) have been lifelong friends. Sadly, Andrew passed away suddenly and unexpectedly a few years ago and is sorely missed.
This was an era where ‘caning’ was still accepted practice although most teachers didn’t. The teachers were fair, some tougher than others and I copped a caning once. I seem to remember deserving it! One of my strongest memories was not my finest moment. My friends and I hid a bottle of Blackberry Nip, the cheapest alcohol around, in the cistern of one of the boarding house toilets. Noone would check there. Of course, when the toilet overflowed the first place the house master checked was the cistern. I’ll never forget the shameful parade to the Headmaster, nor the memory I have of my father’s stern face when he collected me at Queenstown airport when I was suspended for a week. He never once referred to the incident. He knew I’d already learnt my lesson. Instead we went fishing together so it has become a fond memory. My personal experience and our belief that Friends’ School students are community inspired, able to think for themselves and well-adjusted individuals led to Friends’ being the clear choice for Alison and me to send our children to continue their education.
Did you always intend to study Medicine?
It was natural that I would continue with my friends on to university in Hobart, but it wasn’t as I’d hoped. Having grown up with my father who was a surgeon I wanted to study Medicine but despite achieving the pre-requisites, I didn’t make the quota. In many ways, this ‘failure’ spurred me on. Instead I studied Science and went on to study a Master’s Degree in Clinical Biochemistry in Perth all the while reapplying for Medicine. My father died whilst I was undertaking my Science Degree and living at Christ College. It was a tough time, but I had my friends around me. My memories of Dad saying something like, “many people give up what they want without understanding or realising how close they were to success when they gave up” spurred me to keep applying. Persistence paid off, or perhaps the Medical Faculty were sick of reading my annual applications(!) but at any rate I was accepted as a lateral entry student into second year Medicine in 1980. I was 24.
Acceptance was one thing, but survival quite another. I worked at Salamanca Pathology in the evenings and occasional weekends as a Biochemist but was eating through my savings. One day I walked into the clinical school and saw a poster, “Are you sick of fighting for survival? Join the Royal Australian Air Force Undergraduate Programme”. It led to a complete change of direction.
In the RAAF, as at Friends’, I had a fantastic community and learned valuable life skills which have helped me enormously throughout my medical career. I achieved immense personal satisfaction in the RAAF, undertook exceptional training and was involved in operational deployments and experiences which challenged me both physically and mentally. These also provided me with great opportunities to extend myself, take on responsibility, develop leadership skills, improve resilience and learn to work efficiently within a team.
My most rewarding deployments were to assist in humanitarian aid during the Bougainville Crisis, the East Timor conflict and Banda Aceh. These gave a sense of the true meaning of stewardship. The aeromedical response following the Boxing Day Tsunami in Banda Aceh in 2004 had the most profound effect on me. My “life’s bank” of experiences and training were all needed for me to function and provide service in the face of overwhelming humanitarian need. The scale of destruction and loss of life meant our team members were challenged to limits never encountered in civilian life. Our youngest child, James, who is currently in Year 10, was 6 months old.

Tsunami
These memories help to keep me grounded when bureaucracy threatens to overwhelm. They also serve to remind me that we are very privileged to live and work in Tasmania. I decided in 1993 to leave the permanent Airforce to undertake Specialist Anaesthesia training and I haven’t looked back. The following year I met my wife, Alison, who at the time was a senior cardiothoracic intensive care nurse. I remained on the RAAF Reserves for many years which gave me the deployment opportunities I have previously described. I love Anaesthetics. It reminds me a lot of flying, my other passion. There is significant prior assessment and planning to ensure the safe delivery of anaesthesia. Generally, the most challenging aspects are the induction (take-off) and emergence (landing). We are caring for patients at their most vulnerable and it is a great responsibility but also, an honour to care for them.
You are currently Clinical Director, Surgical and Perioperative Services at the Royal Hobart Hospital. What does this role entail?
After 12 years as Director of Anaesthetics and Intensive Care in Burnie, our family moved to Hobart where I took on the role of Director of Anaesthetics at The Royal Hobart Hospital. Currently, I am clinical (medical) director of the Surgical and Perioperative Surgical Stream. My role (working with the Nursing Director) is to direct the clinical operational and strategic activities of Surgical Services, meeting regularly with surgical heads of specialist departments to allocate human and financial resources, provide clinical leadership and ensure the highest standards of service delivery to surgical patients and their families. It is not a role I ever imagined for myself but I’m privileged that it allows me to continue to manage patients in a role utilising my learned skills to provide clinical leadership and governance as part of a team in a large and complex multidisciplinary medical organisation that also teaches our next generation of medical and nursing staff. Within this role I am also fortunate to continue to be able spend time each week giving anaesthetics and being involved in direct patient care.
Has your work been impacted by the COVID-19 pandemic? What can we learn at this time; skills, knowledge, teamwork?
Similar to the school environment, it has been a rapidly changing landscape in the health care sector. The impact of the COVID-19 pandemic in medical facilities across the world has led to tremendous upheaval. In Australia we have been very fortunate to be able to learn from the experiences of our international colleagues via webinars thereby making complex and evolving changes quickly and effectively. Public health directives including social distancing to “flatten the curve” and the fact that we are an island state within an island country has spared us the medically overwhelming catastrophic scenario we were expecting. Nonetheless, a great deal of time has been spent both in preparation for caring for multiple infected patients and caring for our staff including prevention of an outbreak at the hospital. Here are a few examples of what has been achieved. We have transitioned to electronic medical consultations for patients who do not absolutely have to attend clinic appointments, stemmed locum staff movement, closed the hospital to all but essential visitors, utilised staff familiar with disease outbreaks and those with military experience to plan and coordinate training for protective patient care and use of personal protective equipment, allocated one theatre specifically for COVID or suspected COVID patients and set up a designated ward in which to care for them, limited elective surgery, stringent separation of patients arriving in the Emergency Department based on symptoms, redeployment of staff to update skills in areas such as Emergency and Intensive Care to utilise as needed and avoiding face to face meetings or utilising large lecture theatres to hold essential meetings etc. Similar to government briefings we have been holding COVID planning meetings on a daily basis involving multidisciplinary teams including Infectious Disease Specialists, medical and nursing specialties, allied health, administrative staff, cleaners, food services to name a few. Part of my role in conjunction with other senior medical and nursing colleagues in this crisis has been to provide tertiary hospital capability. This means we must continue to treat emergencies as they arise and provide optimal care. It has been particularly challenging to arrange for the safe transfer of patients coming from the North West region for more complex care or surgery during the outbreak. This has required high levels of communication and precise planning between retrieval co-ordinators, ambulance, medical staff etc. It is heartening to see that the measures put in place statewide have seen the number of cases drop so quickly. It has been inspiring to see colleagues rise to the challenge in these difficult times. We have certainly banded together to face this challenge head on. I am very optimistic about the future. We will get through these difficult times and are ready for the possible re-emergence of the virus and do not underestimate its lethal capacity. Our continued commitment to strict hand hygiene and physical distancing measures will save lives.
What have you learned about yourself, and our community, since this pandemic began to affect all of our lives?
We are a global community connected by almost instant information. COVID-19 has impacted us all like no other single event in our lifetime. I have learned that in this crisis there has been the will by the Australian community to adopt the measures put in place by our governments and Chief Medical Officer. It demonstrates how adaptable and resilient we really are. I believe flexibility and adaptive capability are crucial at a time when events are unfolding rapidly; in our homes, workplaces and communities. Our leaders need to be able to adjust to a new reality and not be afraid to make difficult and unpalatable decisions. In the hospital we must work in collaboration and be engaged with colleagues and staff being mindful of the utmost importance of clear and widespread communication. We must learn and rapidly assimilate new information to assist in rapid response when needed. Resilience and leadership skills, developed through my schooling and military life have held me in good stead and given me the capacity to meet this challenge. It has been particularly wonderful to see how community members have looked out for one another during this time, providing help to the elderly in particular. Like others I have been amazed how businesses have adapted and re-invented themselves in order to continue to operate in this new world. And while we would all like to come together as we did before, it is wonderful that we have been able to harness technology to continue to communicate, undertake schooling and to some extent continue to work.
What message can you give our Class of 2020 who are completing their studies in significantly different circumstances and will graduate into a very different world?
Have courage! Yes, your generation is living at a time of great change and challenge. What is important is, what can be learnt from this experience? Having assimilated the lessons and experience of the last few months my advice is this:
- Recognise what is most important in life; health, family, friends and house/home.
- Take every opportunity to pull back from constant over-stimulation and stress. Take time to reflect and simplify life.
- Embark on a pathway that you think will be stimulating and enjoyable but don’t be afraid to change direction if it doesn’t turn out that way.
- Take responsibility, be accountable for your actions and loyal to friends and colleagues.
- Demonstrate optimism.
- Don’t be afraid to stand up and be proactive. Anticipate events with contingency plans, it’s critical leadership competency.
and finally….
Remember the words of Heraclitus, “There is nothing permanent except change”.
